When it comes to cancer, it might be all about rooting out the trouble-makers.
A researcher in the engineering degree program at Southern Illinois University Carbondale just received a grant aimed at helping him develop the means to search out and destroy so-called “cancer stem cells,” which are responsible for regenerating tumors. Farhan Chowdhury’s research will focus on the role these trouble-makers play in one of the deadliest of cancers: pancreatic cancer.
What’s an engineer doing studying cancer?
Pancreatic cancer presents an especially tough challenge for oncologists. It usually is detected late, and surgery often is not an option. That leaves just radiation and chemotherapy as treatment choices. The survival rate for such cancers typically is not promising.
But as he was finishing up his doctorate work, Chowdhury became interested in the mechanical forces involved in cancer and its effects on the body. Tumors, for example, contain varying degrees of stiffness and softness throughout their mass. These forces – stiffness and softness – affect the way body responds to the tumor.
Based on his earlier research on self-renewing stem cells, he demonstrated that such forces also played a role in how and what kinds of cells developed within the tumor. This raised the possibility of weeding out those few trouble-makers, the ones that lay low to survive chemotherapy and then regenerate tumors, to be specifically targeted for destruction by new therapies on the horizon.
A pioneering new approach
In a healthy body, stem cells rejuvenate our bodies by growing new cells. But so-called “tumor-initiating cells” grow cancer in the forms of tumors, which are masses of flawed cells that cause various problems as they grow.
A tumor typically has different parts and different kinds of cells. The tumor-initiating cells tend to be low in number and resistant to chemotherapy, which decreases its effectiveness. But if those cells with such tremendous ability to self-renew could be specifically targeted, it would open up new channels to treat such deadly cancers.
That’s where Chowdury’s method comes in.
“If you think about these cells, they are very happy and grow very well in very soft environments within a tumor,” said Chowdhury, an assistant professor of mechanical engineering and energy processes at SIU. “We don’t really know for sure which cells reside where in the tumor. But ideally, if we could take those cells out and put them on a very soft matrix, the majority probably will not grow, except for these trouble-maker cells. They would grow there.”
Using established human cancer cell lines that are grown in laboratories for research purposes, Chowdhury hopes to create the ideal environment for the trouble-makers to grow. He theorizes that because such cells are so eager to grow, only they, and not the other cancer cells, will do so when placed in a fibrin matrix that simulates a tumor’s softer areas.
One of the key aspects to the research is Chowdhury’s expertise in creating these simulated tumors to make the cells feel right at home.
“So this method would isolate this subpopulation of cancer cells within the matrix,” Chowdhury said. “The mechanical stiffness of the environment is the key to isolating these rogue cells.”
Picking the lock
The walls of cells act much like a lock, with only certain proteins and enzymes acting as “keys” that allow entry. Once the rogue cells are isolated, researchers can study how to “pick the lock,” potentially using those keys to carry drugs directly to and specifically inside them to kill them.
“Once those cells are isolated using this method, they can be studied closely to find their weaknesses,” Chowdhury said. “These guys are responsible for the entire tumor, so if we can figure out how to target them, the entire tumor will die. It would arrest the cancer.”
To do this, researchers will sequence the cells’ RNA in order understand its transcriptional network. The study calls for using next-generation genetic sequencing to learn everything about what makes such cells tick. It’s a massive set of data – big data – and it will require substantial time and computing power to analyze.
“Instead of simply identifying various genetic markers, we want to learn everything that’s being transcribed in that cell,” Chowdhury said. “Once you know the whole transcription, then you can compare that to the other cells to see how they differ or are similar.”
Once the analysis is complete, the researchers can look at various surface makers – unique proteins that are expressed by the cell that are also known as biomarkers.
“If you know them, you can target them to get them to take something inside. It’s like a lock and key,” he said. “It’s like learning their vulnerability, which can then be exploited to deliver targeted drugs.” Such drug therapies might be delivered via carrier protein, nanoparticle or liposome delivered by an intravenous line or needle.
The future holds promise
Such methods remain futuristic for the moment, but Chowdhury’s work promises to be an important building block in creating so-called “personalized medicine,” which theoretically would take a person’s individual DNA into account when exploring various treatment options and drug therapies.
“Every patient is different, and every cancer is different. We are working toward one day personalizing and fine-tuning the treatment based on various factors,” Chowdhury said.
Another part of the study involves using various scientific instruments to help improve early detection of such cancers
Yearlong effort
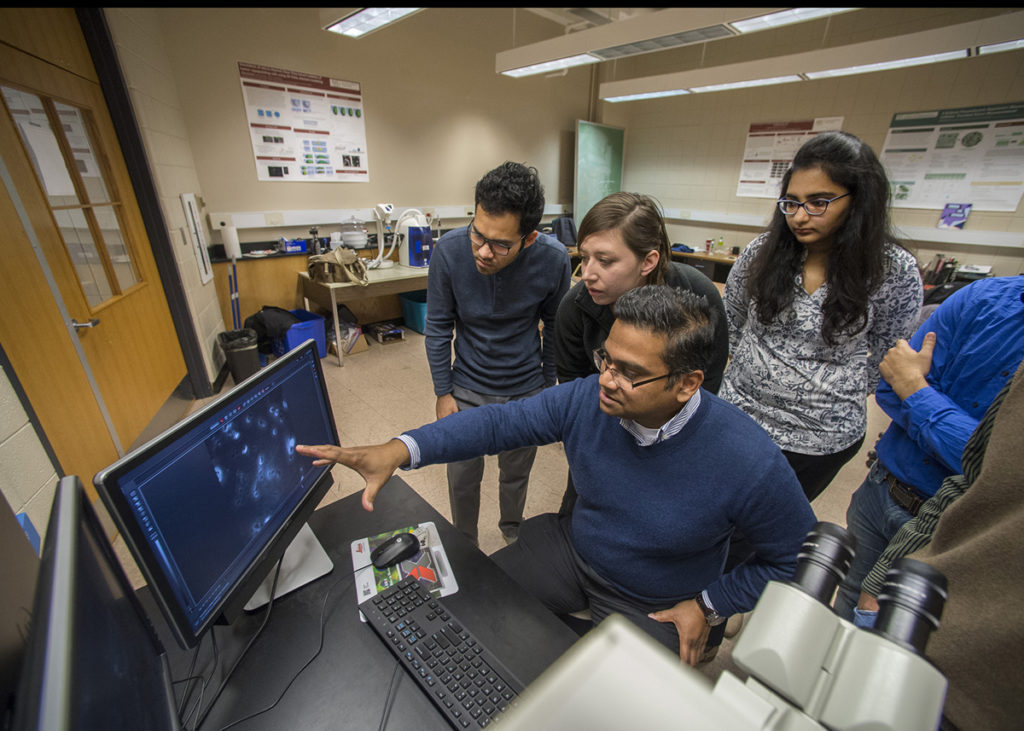
Chowdhury’s $157,000 grant, funded by the Elsa U. Pardee Foundation, will run throughout 2019 and involve at least two graduate students. He also will cooperate with Poopalasingam Sivakumar, his co-primary investigator on the project and an assistant professor in the physics degree program, who will conduct related laser spectrometry analysis. Some of the money also is earmarked for off-site RNA sequencing and purchasing lab supplies and cell lines.






